Cavernous Sinus Thrombosis
Other signs are:
Differential diagnosis:
Lab findings:
Procedures:
ER care:
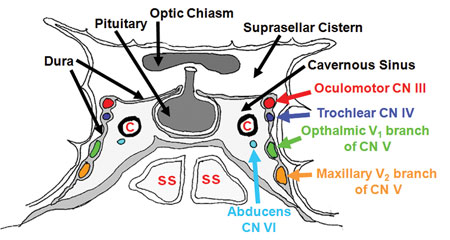 |
| Cavernous Sinus Location and Important Relations |
Location:
1. Lie on the either side of sella turcica
2. Posterior to the optic chiasma
3. At the base of the skull
4. Connection exist between two sinuses
Veins are connected to the sinuses:
Blood comes to the cavernous sinus from the following veins:
1. Facial vein
2. Superior and inferior opththalmic veins
3. Sphenoid and middle cerebral veins
Cavernous Sinus Empty into:
1. Superior and inferior petrosal sinuses.
2. Sphenoid sinus
3. Internal jugular vein.
Labirinthine vien is also connected to the inferior petrosal sinus:
Veins are valve less so blood and infection flow to the either direction.
More favorable sites from where infection can travel to the cavernous sinus are:
Nose
2. Tonsils
3. Orbit
4. Paranasal sinuses
5. Teeth
Other important relations are:
Structures which lie inside the sinus are:
1. Internal Carotid artery with sympathetic plexus
2. Abducent nerve ( VI ) nerve supplies lateral rectus muscle:
Structures embedded in the lateral wall are:
1. Opthalmic nerve (The ophthalmic nerve supplies branches to the cornea, ciliary body, and iris; to the lacrimal gland and conjunctiva; to the part of themucous membrane of the nasal cavity; and to the skin of the eyelids, eyebrow, forehead and nose)
2. Maxillary nerve ( Its function is the transmission of sensory fibers from the maxillary teeth, the skin between the palpebral fissure and the mouth, and from the nasal cavity and sinuses)
Structures attached to the lateral wall are:
1. Occulomotor ( supplies extraocular muscles except lateral rectus and superior oblique )
2. Trochlear ( supplies superior oblique muscle )
Signs and symptoms:
A patient who presents with headache and any cranial nerve findings should be potentially evaluated for CST.
Other signs are:
1. Patient may have associated sinusitis or mid-face infection:
2. Clinical signs and symptoms occur due to venous obstruction and involvement of cranial nerves.
3. Head ache ( usually confined to area supplied by ophthalmic nerve and maxillary nerve )
4. Periorbital findings ( periorbial edema, orbital pain)
5. Visual disturbance
6. Specific cranial nerve signs.
7. Lateral rectus involvement of the contralateral eye indicates bilateral involvement.
8. Within 24 – 48 hours infection spread to contralateral eye through communicating channels.
9. The patient rapidly develops mental status changes including confusion, drowsiness, and coma from CNS involvement and/or sepsis. Death follows shortly thereafter
Other signs are:
1. Periorbital edema, (earliest )
2. Chemosis
3. Lateral gaze palsy ( paralysis of lateral rectus due to involvement of abducence nerve )
4. Ptosis
5. Mydriasis
6. Eye muscle weakness ( oculomotor nerve )
7. Increase retrobulber pressure may lead to exopthalmos or ophthalmoplegia,
8. Increase IOP leads to decrease visual acuity and loss of vision due to optic nerve or central retinal artery traction
9. Hypo or hyperesthesia in the dermatomes of ophthalmic or maxillary nerves
10. Contralateral signs ( bilateral involvement )
11. Menigeal involvement signs:
a. Kerning’s sign: is positive when the thigh is bent at the hip and knee at 90 degree angles, and subsequent extension in the knee is painful (leading to resistance). This may indicate subarachnoid hemorrhage or meningitis.
§ Brudzinski’s sign: patient lie in supine position:
§ The symphyseal sign, in which pressure on the pubic symphysis leads to abduction of the leg and reflexive hip and knee flexion
§ The cheek sign, in which pressure on the cheek below the zygoma leads to rising and flexion in the forearm.
§ Brudzinski's reflex, in which passive flexion of one knee into the abdomen leads to involuntary flexion in the opposite leg, and stretching of a limb that was flexed leads to contralateral extension
The Brudziński neck sign or Brudziński's symptom is a clinical sign in which forced flexion of the neck elicits a reflex flexion of the hips. It is found in patients with meningitis,subarachnoid haemorrhage and possibly encephalitis.
· Systemic signs indicative of sepsis are late findings. They include chills, fever, shock, delirium, and coma.
Causes:
Infections at the sites of venous drainges:
Diabetics are at higher risk.
Differential diagnosis:
· Cellulitis
· Epidural and Subdural Infections
· Epidural Hematoma
· Glaucoma, Acute Angle-Closure
· Orbital Infections
· Periorbital Infections
· Sinusitis
· Subarachnoid Hemorrhage
· Subdural Hematoma
Lab findings:
1. Not specific
2. Leuckocytosis
3. CSF examination
4. Blood cultures
5. D dimmers ( to differentiate from CSVT )
Imagings;
CT and MRI:
CT and MRI:
MRI with MRV and MRI with contrast is preffered. MRV will show absence of blood flow in affected sinus:
CT scan without contrast will show hyperdense shadows , CT with contrast appreciates better.
Carotid angiography.
Procedures:
· Lumbar puncture may be helpful in distinguishing CST from more localized processes (eg, sinusitis, orbital cellulitis). Lumbar puncture reveals inflammatory cells in approximately 75% of cases.
ER care:
1. Aggressive broad spectrum, IV antibiotic therapy.
2. Anticoagulent ( with care )
3. Locally administered anticoagulants ( for experimental and refractory cases )
4. Corticosteriods ( surgery )
5. Surgery ( difficult and rarely beneficial )
Complications
· Meningitis
· Septic emboli
· Blindness
· Cranial nerve palsies
· Sepsis and shock
Comments
Post a Comment
Post Your Reply and Give Your Opinion About the Post